- Get Certified
- Certification Process
- Subspecialties and FPDs
- Focused Practice Designations
- Anesthesiology Critical Care Medicine
- Emergency Medical Services (EMS)
- Health Care Administration, Leadership, & Management (HALM)
- Hospice and Palliative Medicine
- Internal Medicine – Critical Care Medicine
- Medical Toxicology
- Neurocritical Care
- Pain Medicine
- Pediatric Emergency Medicine
- Sports Medicine
- Undersea and Hyperbaric Medicine
Oral Exam
2025 Administration
| 2025 Exam Dates |
Winter: December 9 – 12 |
|
2025 Registration Periods Deadline: 11:59 p.m. ET, on the final day of the registration period |
Winter: February 20 – October 29 |
| Fee* | $1,255 |
|
LATE 2025 Registration Periods Deadline: 11:59 p.m. ET, on the final day of the registration period |
Winter: October 30 – November 10 |
| LATE Fee* | $1,565 |
* Fees subject to change
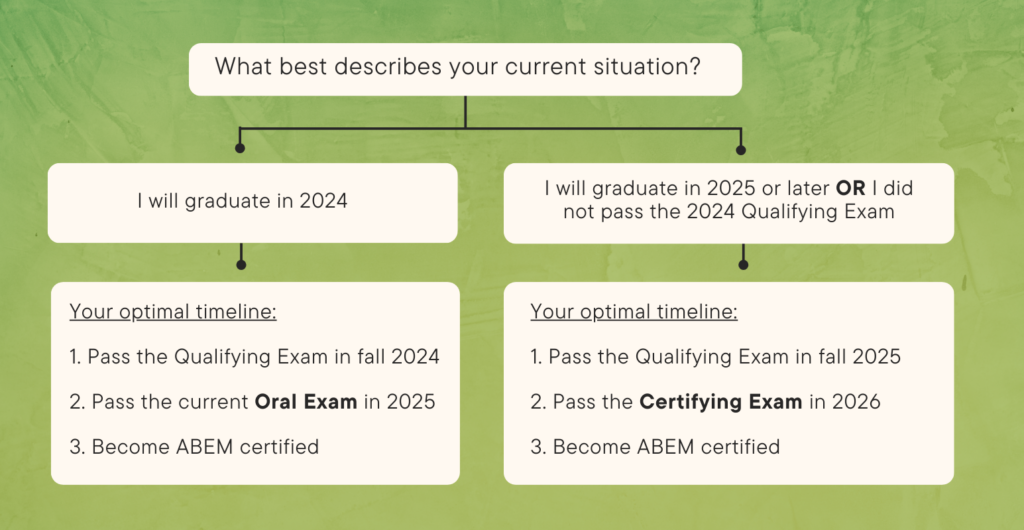
Will I take the Oral Exam or Certifying Exam?
Oral Exam Overview
The third step for ABEM certification is the Oral Certification Examination. The Oral Exam is a standardized test of Emergency Medicine knowledge, using scenarios based on actual clinical cases.
The Oral Exam measures skills that cannot be tested on a multiple choice exam. It’s important that ABEM-certified physicians can clearly communicate with patients and their families, organize information about patients, and make good choices for patient management.